Why successful IVF often requires making multiple embryos for one baby
In vitro fertilization typically takes more than one embryo to safely achieve pregnancy — and unused embryos are often discarded.
Why it matters: Alabama's Supreme Court ruled in February that frozen embryos created through IVF are children under state law, meaning fertility clinics in the state could be held legally liable for disposing of surplus embryos.
- Other states are considering so-called fetal personhood bills.
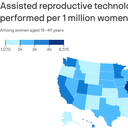
By the numbers: More than 86,000 infants were born in 2021 with the use of assisted reproductive technologies like IVF, according to the most recent CDC data.
- That accounts for 2.3% of all of the births that year.
More than 202,000 embryo transfers were performed to get that number of infants.
Between the lines: IVF patients usually need multiple embryos to ensure just one healthy baby, because the process often involves embryo attrition, Lucky Sekhon, reproductive endocrinologist and infertility specialist at RMA of New York, tells Axios.
- Many of the embryos used in IVF are frozen, and first have to be thawed before getting transferred — a process that not all survive.
- Not all thawed embryos pass genetic testing and are considered to have high reproductive potential.
- Not all embryos of high reproductive potential successfully implant into the uterus.
- And not all embryos that implant lead to a healthy baby — pregnancy loss is possible.
Three or more embryos may be required for a patient to have one pregnancy, Sekhon says.
- Of the embryos that thaw and pass genetic testing, about half to two-thirds lead to pregnancy in an ideal scenario, she says.
IVF patients can choose not to discard their unused embryos, but other options may not be a fit for everyone, particularly if people have embryos that are graded unlikely to lead to a healthy pregnancy.
Reality check: If laws prohibit clinics from discarding embryos, this could increase the time, cost and physical and emotional toll it takes to get pregnant via IVF.
- Clinics could be deterred from storing multiple embryos, and that could lead to clinicians retrieving and fertilizing fewer eggs per cycle, Sekhon says.
- With fewer eggs retrieved and fertilized per cycle, that could mean patients have a higher probability of needing more egg retrievals to be successful, she says.
- And if patients had to store all extra embryos indefinitely — including those that had low chances of resulting in a healthy pregnancy — those costs would add up.
Bottom line: Without the ability to discard surplus embryos, IVF — already expensive and out of reach for many — could become even less accessible.