States clamping down on coverage of weight-loss drugs
States are tightening access to blockbuster weight-loss and diabetes drugs to protect against the pricey treatments from blowing up their budgets.
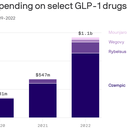
Why it matters: State employee health benefits and Medicaid programs have seen a surge in costs from a class of drugs known as GLP-1 agonists. With limited taxpayer dollars at hand, some state officials say they have no choice but to clamp down amid the drugs' soaring popularity.
- Health plans generally cover GLP-1s like Novo Nordisk's Ozempic or Eli Lilly's Mounjaro for diabetes. But when it comes to weight loss, states are adding limits on how patients can get them, hiking copays or in some cases, dropping coverage of the drugs altogether.
Driving the news: In North Carolina, a state board recently decided the health plan for 750,000 state employees would no longer cover GLP-1s for weight loss. Officials found spending on the drugs would have exceeded $170 million this year.
- Spending on the 22,000 weight-loss patients who were treated with a GLP-1 was equivalent to the cost of providing a 4% retirement bonus lawmakers had mandated for 250,000 retired state employees, according to treasurer Dale Folwell, who oversees the state health plan.
- "Our state health plan is under siege because of the cost of this one type of drug," Folwell told Axios. "If we had stayed the course, there was a potential doubling of the premium on state employees."
Zoom in: North Carolina is among several states grappling with how to handle coverage of these drugs for their workforces.
- Delaware officials are considering changes after finding costs are growing far faster than expected.
- Connecticut, which has 250,000 state employees and has seen a roughly 50% jump in GLP-1 spending every year since 2020, began a pilot requiring employees to participate in a clinical lifestyle management program if they were prescribed the drugs. The program, run by an outsourced provider, offers personalized weight management help.
- "We are starting to see a flattening of the cost curve," state comptroller Sean Scanlon told Axios.
- The jury is still out on the program, he said. While costs are still increasing, "we're not projecting another 50% increase."
Between the lines: State Medicaid programs that cover far more people are also grappling with rising GLP-1 costs.
- A limited number of states — 16 in all — provide coverage of any sort for weight-loss medications, according to a 2023 KFF survey of Medicaid directors.
- Medicaid directors of those states said they had tight restrictions on the drugs. These included requiring patients to have certain body mass indexes and additional health conditions to qualify for coverage, said Liz Williams, a senior policy analyst with KFF's Program on Medicaid and the Uninsured.
The intrigue: Coverage restrictions may save state budgets, but they could face pushback from patients who say they're unfairly blocking access to highly effective treatments for obesity.
- Already in Washington, a state employee last fall filed a lawsuit challenging the state's ban on covering weight-loss drugs.
The bottom line: Scanlon, the Connecticut comptroller, said he believes the drugs in the long term will pay off through better health outcomes. But it's not an easy calculation to make, he acknowledged.
- "I look at like: Your costs are going up no matter what. Do you want to make your costs go up less? I think the answer to anybody in my position is probably yes."